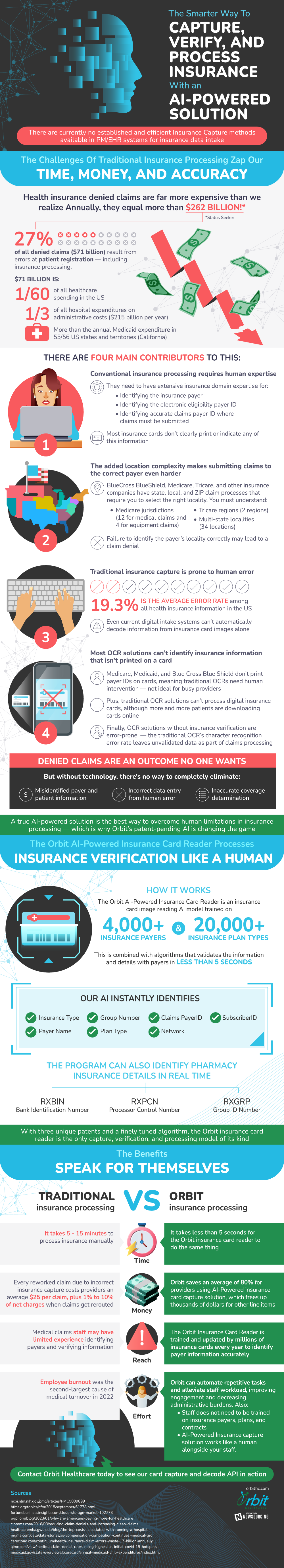
Artificial intelligence (AI) has the incredible ability to mimic the human ability to learn. It can be trained through large data sets to recognize patterns and analyze data to create predictions. A lot of industries are poised to benefit greatly from this technology, and the healthcare insurance industry is no exception, especially within the claims submission process. Currently, a large amount of claims are being rejected, which is costing an astounding $262 billion yearly. Errors in the patient registration phase account for 27% of this amount, which totals $71 billion.
A lot of these errors are a result of the insurance processing industry’s reliance on human expertise. Workers are required to manually identify critical data, including insurance payer and electronic eligibility payer ID, due to the fact that this information is not located on insurance cards. Human interpretation is not always perfect- in fact, there is a 19.3% error rate for health insurance data. AI has the ability to limit these errors through its highly accurate validation process. It can also complete this process in five seconds, which is a massive improvement from the fifteen minutes that manual processing can take. By implementing AI, health insurance card processing with AI can be submitted more accurately and efficiently.
Source: OrbitHC
